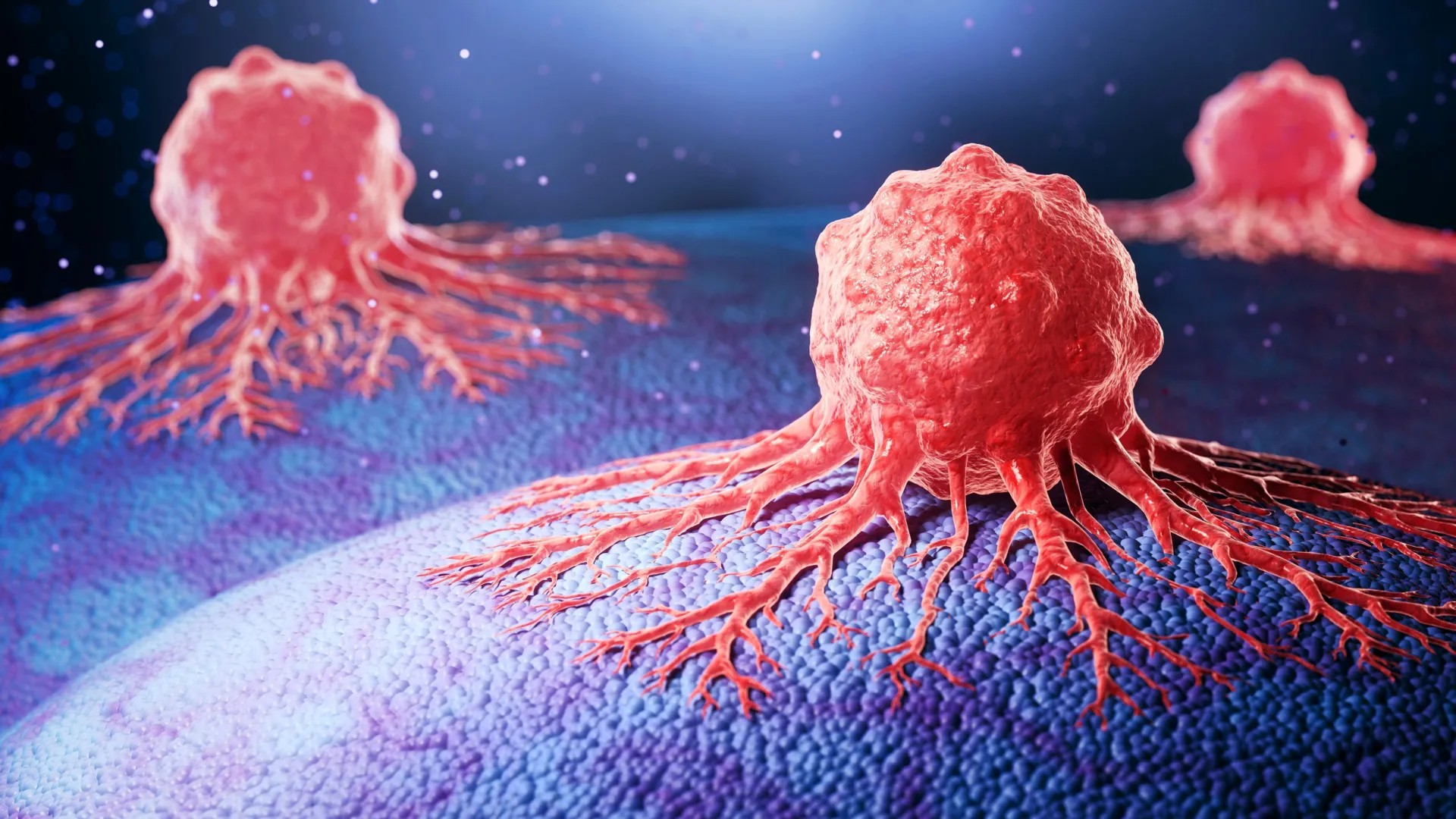
Pancreatic cancer remains one of the deadliest forms of the disease, with survival rates lagging behind many other cancers. A new study reveals a critical mechanism driving its aggressive spread: pancreatic tumors don’t just grow; they actively reprogram surrounding healthy tissue to support their invasion. This explains why the cancer is so difficult to contain once it starts spreading.
The Silent Invasion: How Cancer Co-Opts Healthy Cells
The study, led by researchers at the Center for Research on Inflammatory Diseases (CRID), found that pancreatic tumors manipulate the tissue around them, turning it into an ally. Specifically, the tumors stimulate cells to produce large amounts of a protein called periostin, which reshapes the structural framework of healthy tissue – the extracellular matrix – making it easier for cancer cells to break through and reach nerves.
This process, known as perineural invasion, is a hallmark of pancreatic cancer’s aggressiveness. Cancer cells travel along nerves like highways, rapidly expanding into other parts of the body. The researchers used advanced gene analysis to map exactly how this happens at a cellular level, integrating data from dozens of tumor samples with unprecedented precision.
Why Treatment Fails: A Fortified Tumor Environment
The reshaping of the tissue around the tumor doesn’t just aid invasion; it also creates a physical barrier against treatment. The tumor environment becomes dense and fibrous, a phenomenon known as the desmoplastic reaction, making it harder for chemotherapy and immunotherapy drugs to penetrate. This protective layer allows cancer cells to survive and continue spreading unchecked.
Worldwide, pancreatic cancer claims nearly as many lives as it diagnoses each year, with approximately 510,000 new cases and deaths reported annually. In Brazil, estimates from the National Cancer Institute (INCA) show about 11,000 new cases and 13,000 deaths yearly. Oncologist Pedro Luiz Serrano Uson Junior notes that only around 10% of patients achieve long-term survival, even with treatment.
The Promise of Precision Medicine: Targeting Periostin
The research team believes that periostin represents a promising new target for therapies. Blocking its activity or eliminating the cells that produce it could limit nerve invasion and slow the cancer’s spread. Clinical trials in other cancers are already testing antibodies designed to block periostin, and researchers hope the same approach could work for pancreatic cancer.
This strategy aligns with the broader trend toward precision medicine, where treatments are tailored to specific molecular changes in a patient’s tumor. Uson suggests that future therapies could focus on preventing the tumor from becoming invasive in the first place.
“If we can develop antibodies or drugs that block these stellate cells, we’ll have tools to prevent the tumor from acquiring this invasive capacity so early,” Uson says.
The study also demonstrates the power of advanced data analysis, extracting new insights from existing research. The next step is to translate these findings into effective treatments that act before the cancer spreads, offering a potential breakthrough in the fight against this deadly disease.